You must be 18 years or older. You must weigh more than 110 pounds. You must be in good health.
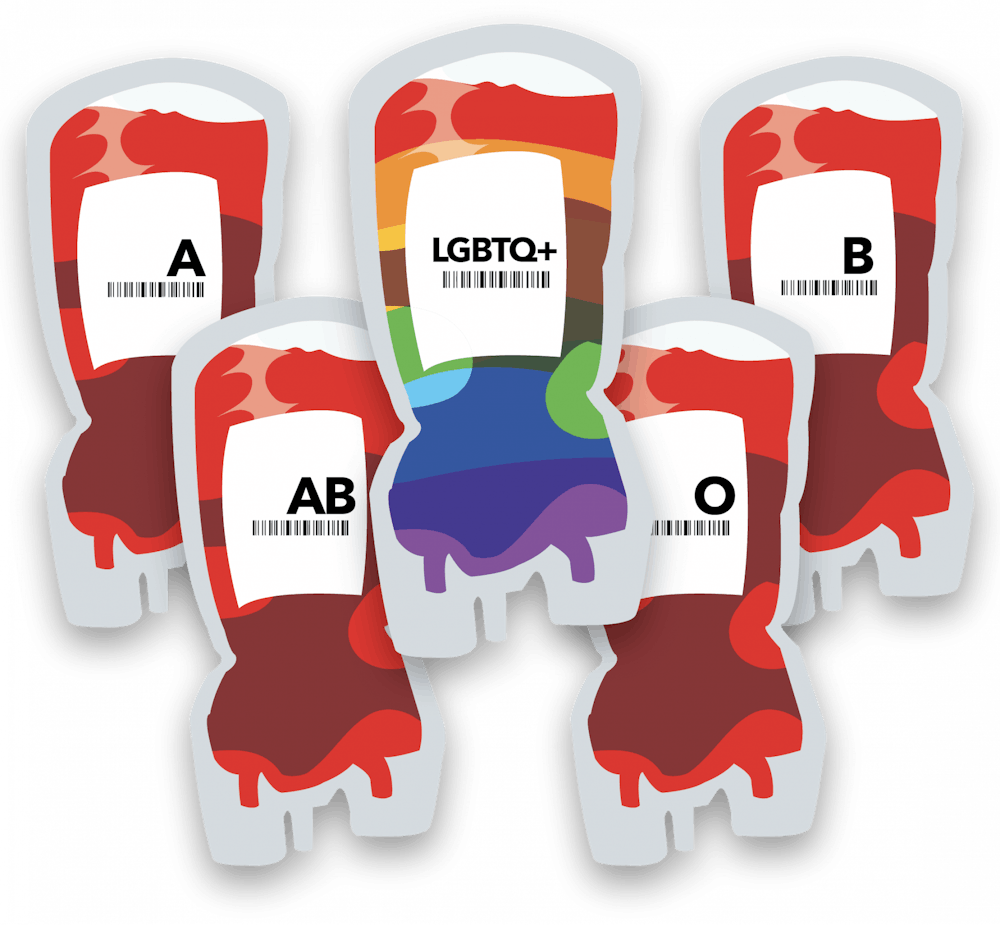
Simple rules for donating blood, right?
Not necessarily.
You must not be a male who has had sexual contact with another male in the last three months.
You may be able to donate blood as a trans man … but not if you’ve had sex with another man in the last three months. If you are an individual who identifies as female and has had sex with a man, you may be eligible to donate blood.
When Kristina Wilson-Pike tried to donate blood at the American Red Cross, the last restriction stopped her from donating, though the restrictions were more severe when she tried to give blood eight years ago.
The transgender woman and retired firefighter wanted to give back to her community, but this opportunity wasn’t available to her.
“It is kind of unfair. We’re talking about my blood going to save someone’s life,” Wilson-Pike said. “As a firefighter, I donated blood a lot, so to find out later I couldn’t donate, it was quite upsetting.”
Today, men who have sex with men (MSM) can only donate at the Red Cross if they are sex free for three months. Due to restrictions from the FDA, this is the same for BioLife, CSL Plasma and many other blood and plasma donation places in the country.
It doesn’t matter if you’re in a monogamous relationship. It doesn’t matter if you’ve never had HIV. It doesn’t matter if you bring in test results. If you’re a man who has had sex with men in the last three months, you cannot donate. At the Red Cross, this also applies to trans men. But that 40-year-old policy may be changing after the FDA announced earlier this year it’s considering loosening the regulations against MSM.
“Why does it matter who I sleep with? What does it matter if I am trying to save someone’s life?” Wilson-Pike, member of MuncieOUTreach, said. “If I am in the hospital, I’m not going to care where the blood comes from.”
Regulations and Reform
In 1983, according to the ADVANCE(assessing donor variability and new concepts in eligibility) Study, the FDA put a policy in place excluding any MSM since 1977 from donating blood and plasma. This restriction came after the AIDS epidemic, when people with HIV passed the virus through blood transfusion. Though there is medicine now that can help treat types of HIV, according to HIV.org, the virus doesn’t have a cure and can cause hepatitis B, hepatitis C, tuberculosis and AIDS.
According to the CDC, though HIV is higher among the LGBTQ+ community, with MSM being the group most heavily affected, heterosexuals made up 22 percent of new HIV infections in 2020, and of that, women accounted for 68 percent.
Despite nucleic acid testing, a test which recognizes HIV in blood, being introduced in the late 1990s and each person’s blood being tested, donation restrictions have been kept in place.
Claudia S. Cohn, chief medical officer at the Association for the Advancement of Blood & Biotherapies (AABB) said this is because of a “window period,” the time after being exposed to HIV but before testing can detect it.
“To help ensure that donors do not unknowingly transmit HIV to a patient during this ‘window period’ … the FDA and AABB require a 3-month waiting period after which donor testing will be able to detect a recent infection,” Cohn said. “Manufacturers of donor testing systems are continually working to improve test performance, including earlier detection of very low levels of the virus.”
In 2015, the policy was updated to allow men who haven’t had sex with another man within a year to donate. Then in 2020, the policy was updated again to shorten the period to three months.
Wilson-Pike said three months doesn’t make a difference because she knows people who have donated who are in same sex relationships and have had sex.
“It doesn’t really matter,” she said. “People are gonna lie, so if they’re testing it anyway, it doesn’t matter.”

“Liquid Gold”
According to the National Library of Medicine, after the one year policy was implemented in 2015, there was no observed significant increase in HIV risk through blood/plasma transfusion. Per 100,000 cases, HIV incidence in first-time donors before the policy was implemented was estimated at approximately three people, and it stayed the same after two years.
According to the Cleveland Clinic, “plasma is the liquid component of your blood that contributes to 55 percent of your blood’s total volume.”
The associate director of communications at BioLife, Mary Ann Schultz, called it “liquid gold,” saying it can “create therapies for hundreds of thousands of people living with rare and complex chronic diseases.” Plasma also helps with nutrients, removing waste, preventing infection and recovering from injury.
Unlike blood donation, a machine separates plasma from the red cells and platelets in blood, then the blood is put back into your body. Plasma replenishes itself in roughly 24 hours, so donors can usually donate about twice a week.
At BioLife, Shultz said the process usually takes about two hours. Potential donors start with a physical examination and a medical screening, and if passed, they move on to the actual donation.
According to Abbott, the plasma supply during the COVID-19 pandemic went down by 20 percent. People were stuck in their homes, unable to donate during the pandemic, and it’s still having an effect. In January 2022, the Red Cross declared their first-ever blood crisis.
The Red Cross supplies 40 percent of the United States’ blood, but they have had to limit their number of distributions since the pandemic. This is one reason why the FDA updated their restrictions on the period MSM can donate.
Wilson-Pike said it shouldn’t take a blood shortage to create change for MSM.
“My biggest thing is take [blood] from everybody, and if it doesn’t test right, then don’t use it. Don’t discriminate blood,” she said. “My basic thing is just it should be that way all the time, not just when they are short on blood. It should be a set standard forever.”
Donating plasma is a popular way for college students and those with lower incomes to make money. According to GoBankingRates, as of December, you could make anywhere between $360 and $1,000 donating, though it depends on the number of visits and the location.
BioLife’s homepage says, “Give plasma and get up to $900,” and CSL Plasma’s website says you can make $100 on your first donation and $500 in your first month. The money at most plasma locations, like CSL Plasma and BioLife, is loaded onto a prepaid card.
Willow Bishop, second-year theatre creation and dance studies student at Ball State University, has been donating plasma twice a week since October 2022 to pay for rent. Though she hasn’t been going as frequently lately, she has already made $1,100.
Wilson-Pike said she is technically homeless right now, and she wanted to donate to make extra cash, but she didn’t want to go through potentially being rejected again.
Wilson-Pike isn’t the only one who is afraid.

The Dread of Denial
Ethan Bravo is the treasurer for Spectrum and a first-year social studies teaching and public history major at Ball State. He said everyone he knows who has thought about donating is either too scared or doesn’t want to “go through the hassle of being deferred.”
MJ Butcher, first-year public history major, said they tried to donate at an on-campus blood drive hosted by the Red Cross last semester, but they were deferred. Butcher said the Red Cross wouldn’t tell them why they were rejected, just that it wasn’t because of their heart condition.
Butcher said though they aren’t sure, they assume it’s either because they’re nonbinary or because they’re gay, questions they were asked in the donation process.
“If they are going to defer you, they need to tell you why,” Butcher, the Spectrum vice president, said. “I don’t see why I would be told no.”
Butcher believes the Red Cross’s eligibility is based more on sexuality than assigned sex since the restrictions say trans men cannot donate (within the three months) but trans women may be able to.
“If you’re thinking purely biologically, trans men and trans women should be reversed in this sort of policy,” they said.
Butcher said there are too many holes you must jump through, making it more difficult to donate.
“Sometimes, I think people in the community are too confused on the requirements that they don’t want to go through the hassle of possibly being denied,” Bravo said.
Bravo thinks blood donation places shouldn’t be worrying about gender identity as much and that everyone should be checked.
“If anyone can contract it, no matter who you are, you can get HIV or sexual diseases,” he said. “They should really reevaluate the questions. I do get sex at birth because that’s biological, gender identity isn’t an important question.”
Butcher agreed, saying that it should be based solely on health and HIV.
“It’s gotten better in the past 30 years, but it’s still not great and can always be better,” they said.

Following Suit
Compared to some of the United States’ allies, the country is behind when it comes to lighter blood donation restrictions.
According to Canadian Blood Services, in April 2022, criteria specific to MSM and sexual behavior-based screening, regardless of gender or sexual orientation, was removed.
In England, Scotland and Wales, according to NHS Blood and Transport, MSM who have had the same partner for three months or longer can donate, and anyone, regardless of gender or sex, who has had anal sex with a new partner within three months cannot donate. This has been in place since 2021.
The Red Cross, OneBlood, Vitalant and Stanford Blood Center, along with the FDA, are working on a study to make donating blood a more inclusive community. The ADVANCE (assessing donor variability and new concepts in eligibility) Study is testing the blood of those with HIV and those in the LGBTQ+ community to see if the restrictions on blood donation are valid. Enrollment ended Sept. 30, 2022, so the study is currently underway.
The Red Cross said they couldn’t say much because of the ongoing process, but they said they are excited about the study and want to make a more inclusive and equitable donation process.
“The American Red Cross seeks to build an inclusive environment that embraces diversity for all those who engage with our lifesaving mission. As such, the Red Cross believes blood donation eligibility should not be determined by methods that are based upon sexual orientation and is committed to working with partners toward achieving this goal.”
The Red Cross said it wants to treat all donors with equality and respect.
Now, the FDA is taking the next step by considering using individual risk assessment (IRA), asking all donors the same questions.
There would be no time-based deferrals for MSM and women who have sex with MSM, According to the FDA. All genders and sexes will be asked about new and multiple sexual partners and a history of anal sex within the past three months. Those who haven’t reported having anal sex with a new partner in the three months will be eligible to donate, assuming other criteria are met as well.
The FDA said it would take 60 days to take comments regarding this change. Afterward, the agency will review the commentary and make a decision.
“The United Kingdom, Canada and many other countries have successfully adopted IRA to evaluate donor eligibility without affecting the safety of the blood supply,” Cohn said.
Rhonda Sciarra, communications director at CSL Plasma, said CSL Plasma is aware of the FDA’s potential change and will comply with the guidance issued.
“CSL Plasma believes all potential plasma donors must be treated with equality, fairness and respect,” Sciarra said. “Accurate donor histories and consistent donor deferral standards are critical to maintaining safe plasma donation and safe plasma-based therapies for patients.”
Butcher, Bravo and Wilson-Pike all said they want to see change regarding these restrictions.
“Helping each other or any community in any way you can is the best thing you can do,” Bravo said. “I would try and go ahead and donate when I can.”
Contact Lila Fierek with comments at lkfierek@bsu.edu.