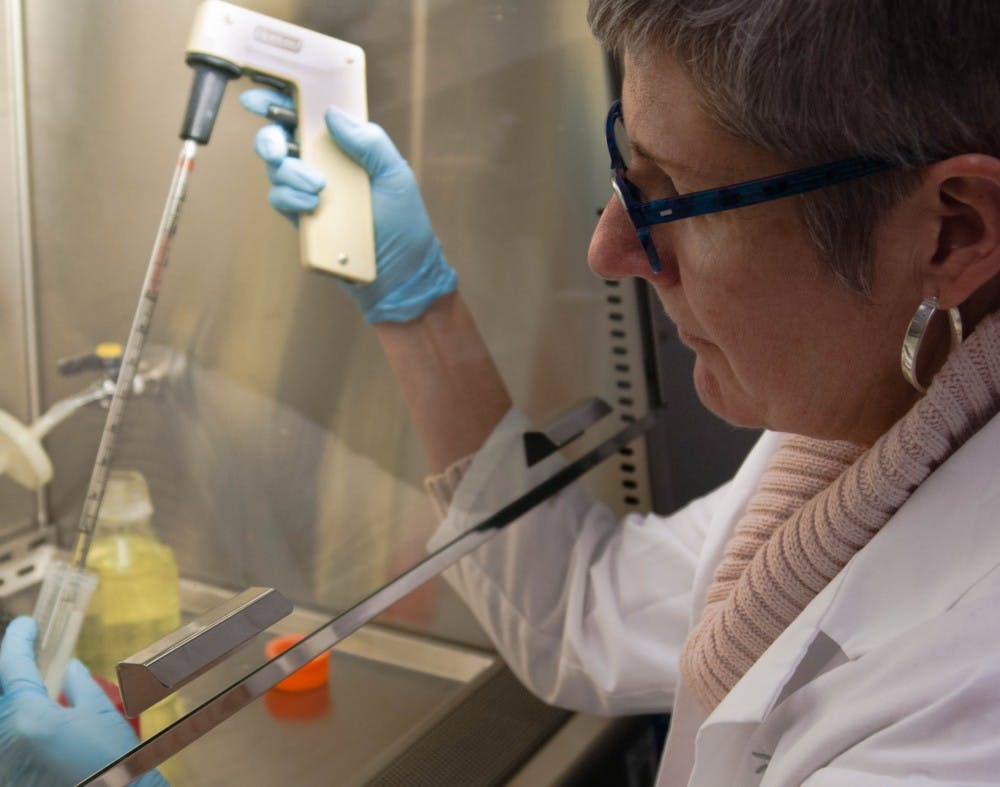
As a child, Vice President of Research Susan McDowell remembers that all she wanted for Christmas was to satisfy her scientific curiosity.
One year, she asked for a microscope. Another year, McDowell said that while “some kids were asking for a soccer ball, I was asking for a chemistry set.”
Now, McDowell is sharing that passion for research and science with students at Ball State.
The research McDowell and her students conduct is centered around the use of alternative medications to antibiotics that treat bacterial infections.
While antibiotics directly affect and kill bacteria, these alternative drugs directly apply themselves to human cells to make them resistant to disease.
Melissa Tinsley, a microbiology major who conducts research alongside McDowell, said the motivation for their studies is the pursuit of the answer to a “bigger question.”
“This bigger question is going to help people,” Tinsley said. “It’s going to either help them in their health, or it’s going to help them with a better understanding of the world.”
In the pursuit of their question, McDowell and her students may have found the answer to treating antibiotic resistance within bacteria.
Over time, bacteria develop an immunity to the antibiotics used to treat them. However, because the drugs used in McDowell’s lab are applied directly to human cells, bacteria never have the chance to make contact and develop a defense to the medication.
Since 2006, McDowell studied how these drugs might be used to treat bacterial infections, including staph infections, without contributing to antibiotic resistance.
Staph infections can often be life-threatening, which was the case for McDowell’s father, Bill McDowell, who contracted a staph infection while in the hospital and died a few days later.
According to a 2011 study published by JAMA Internal Medicine, of the 80,000 life-threatening staph infections that year, more than 11,000 people died from infection — almost enough to fill the seats of John E. Worthen Arena at Ball State.
Staph infections commonly occur at the hospital, and about one in three people are natural carriers of the staph bacteria, according to The Centers for Disease Control and Prevention.
Hospitals have procedures in place, such as washing hands, to stop the spread of the bacteria, but they can’t stop the spread completely.
Of the 11,000 people who died from staph infections in 2011, nearly 30 percent acquired the infection while in the hospital.
Staph bacteria can live for a long time on a variety of surfaces, including the fabric of curtains between hospital beds and on medical equipment, making it almost impossible to keep an area completely sterile.
McDowell’s father went to the hospital for a cold, but while his body was fighting the virus, the staph infection spread and his body began to shut down.
“As I sat there in his hospital room, I knew that they were trying to treat him for staph infection that was resistant to our most common antibiotics,” McDowell said. “He was being treated with antibiotics … and they could not limit the infection.”
Once the infection reaches the bloodstream, the kidney begins to deteriorate trying to clean the infected blood. As a result, other organs begin to shut down.
“It’s a very painful death, and it’s hard to watch someone walk through that,” McDowell said. “Part of what happens is your lungs start to fill up with fluid, and it becomes very, very difficult to breathe.”
Eventually, a patient’s heart is working so hard to keep the body functioning that it gives out.
The death of her father and the work of her students motivates McDowell to continue her research to “help people in the future” so they won’t “lose their loved ones.”
Their work will not only help in the fight against antibiotic resistance, but also aid in the prevention of immunocompromise in groups with weakened or fragile immune systems, such as children and the elderly.
Because of what they have accomplished and how hard they work, McDowell is proud of the work that has been done in the lab and proud of her student researchers.
“My favorite part about working with them is watching them develop as scientists right before your eyes,” McDowell said. “It’s rewarding because I get to pass along techniques that were passed along to me.”
McDowell isn’t just passing on her knowledge of science, however. She is also sharing her enthusiasm for the work that she does with the next generation of scientists and researchers.
“[McDowell] is just extraordinarily passionate and enthusiastic about this research, and it just radiates onto you because she loves it so much,” Tinsley said.
When Tinsley first began to research and work in the lab alongside McDowell, she was unsure whether she wanted to pursue research as a career. However, Tinsley immediately “fell in love with the research” and “fell in love with the bacteria.”
Tinsley describes McDowell as “instrumental” in fostering her interest in research and what she wants to do with science in the future.
“Being in Dr. McDowell’s lab, I have learned far more than I could have ever imagined about how to be successful as a professional,” Tinsley said. “She’s taught me how extraordinarily important science is.”
Moving forward, McDowell is working with the Ball State Innovation Corporation to find a commercial partner who can initiate the next phase of drug development for an experimental medication called ML141 used in the lab.
The drug is currently in an unusable powder form, so a commercial partner is needed to create a consumable tablet of the drug for mass-production.
ML141 also requires extensive safety testing by a corporate entity before it enters the commercial market, but it promises to be a potential answer to the prevention of bacterial infection and a contribution by McDowell and her students in the fight against antibiotic resistance.
Contact Adam Pannel with comments at arpannel@bsu.edu.